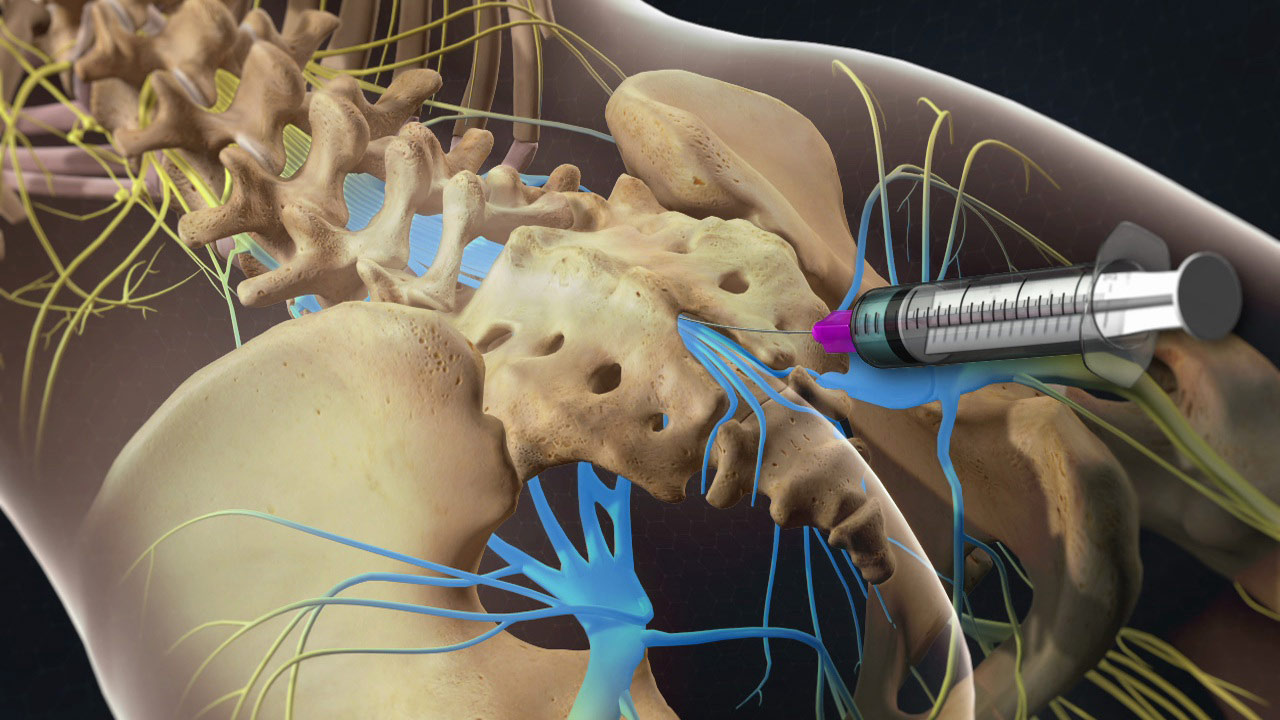
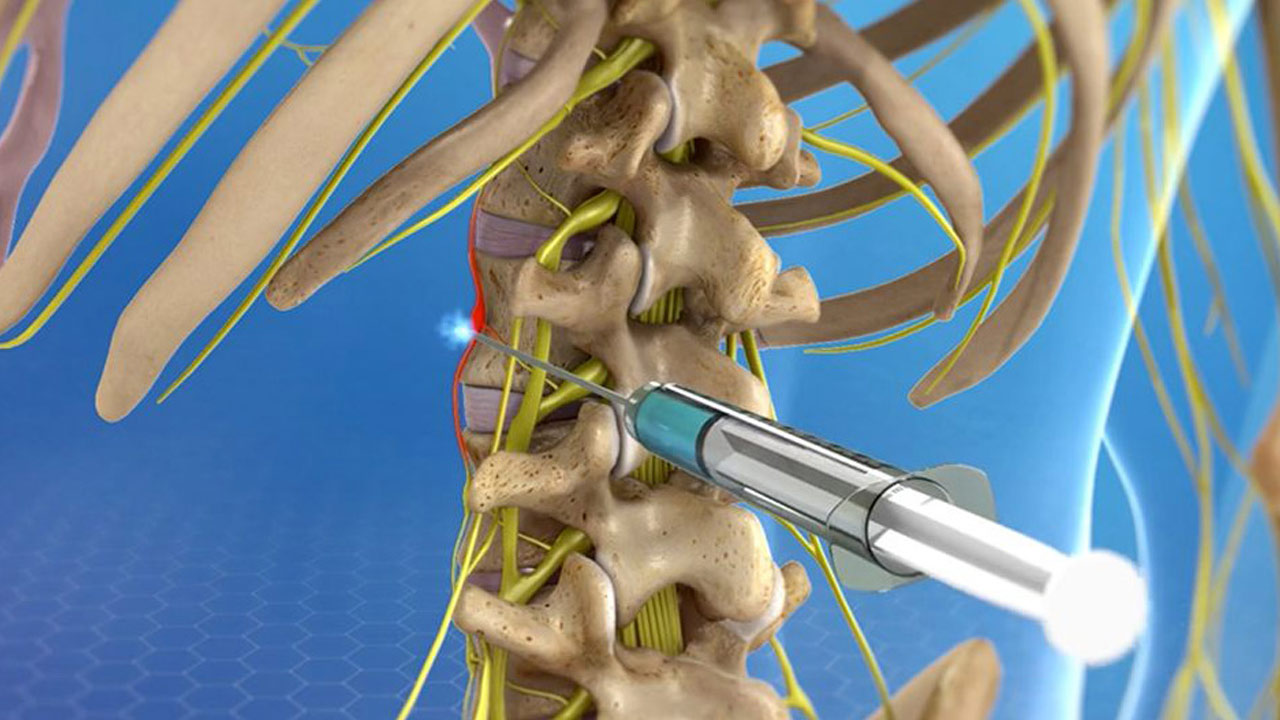
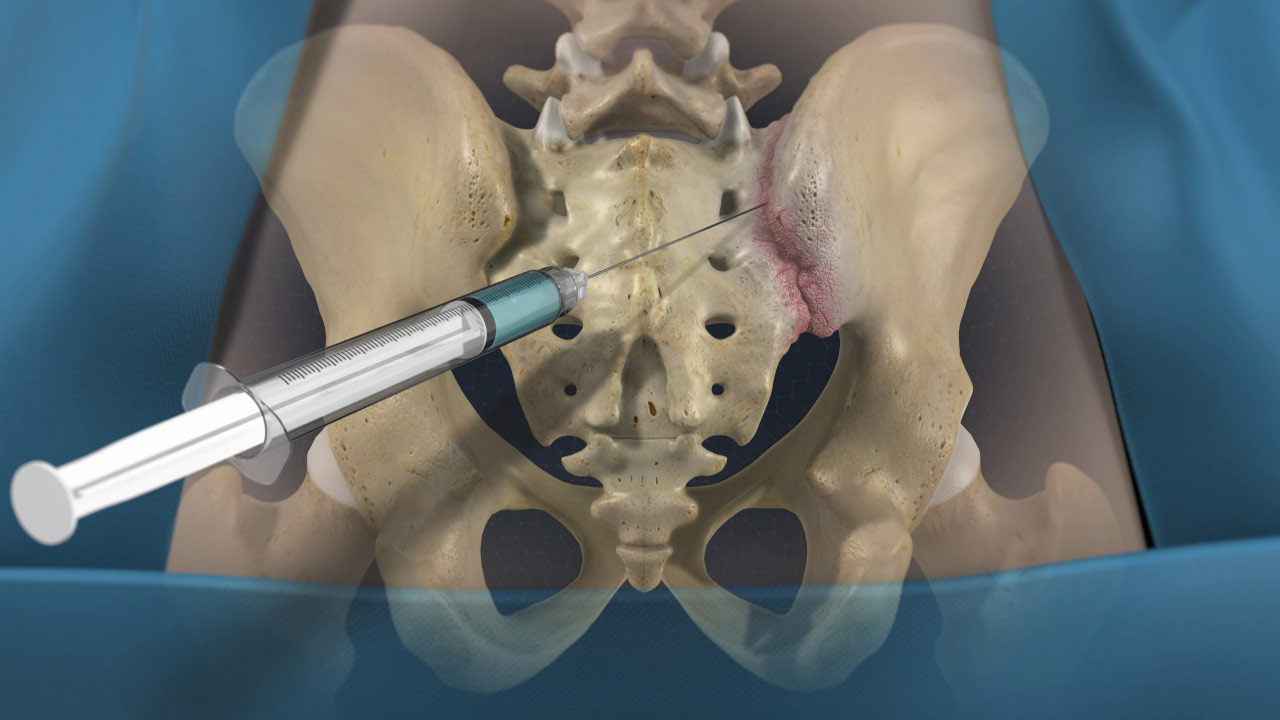
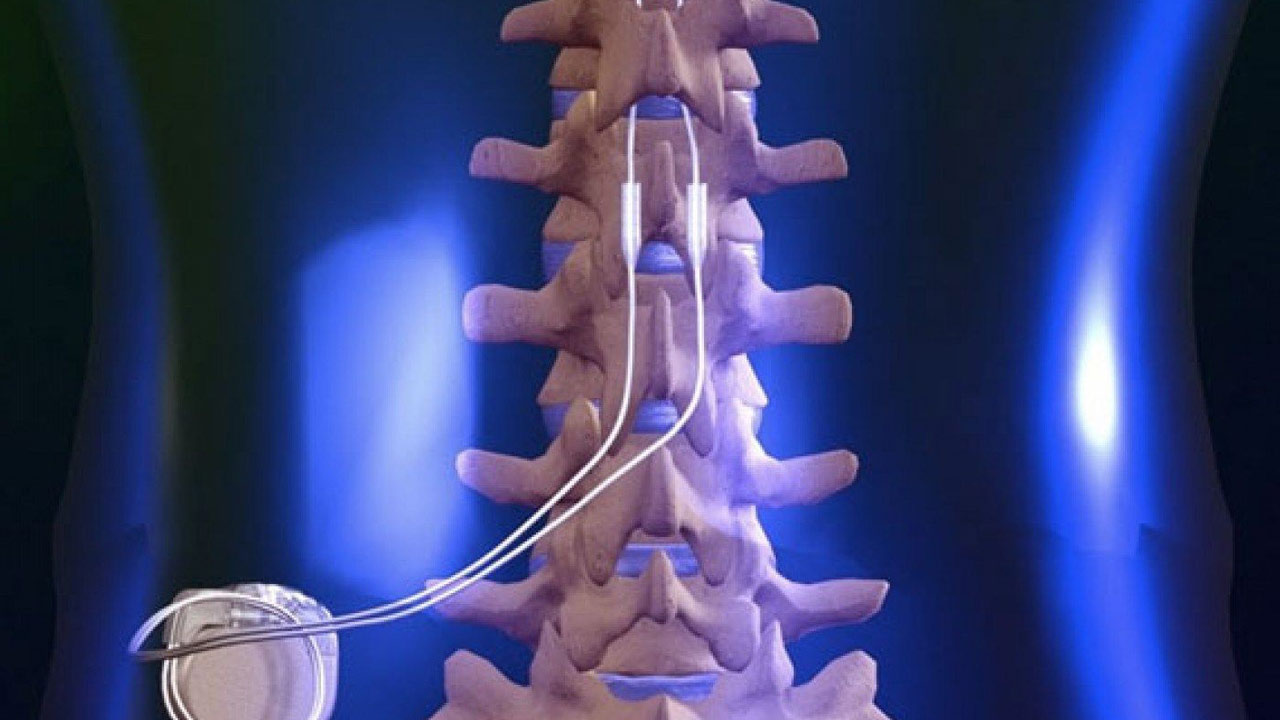
An epidural steroid injection (ESI) is a minimally invasive procedure that can help relieve neck, arm, back, and leg pain caused by inflamed spinal nerves due to spinal stenosis or disc herniation. Medicines are delivered to the epidural space, which is a fat-filled area between the bone and the protective sac of the spinal nerves. Pain relief may last for several days or even years. The goal is to reduce pain so that you may resume normal activities and a physical therapy program.
A steroid injection includes both a corticosteroid (e.g., triamcinolone, methylprednisolone, dexamethasone) and an anesthetic numbing agent (e.g., lidocaine or bupivacaine). The drugs are delivered into the epidural space of the spine, which is the area between the bony vertebra and the protective dura sac surrounding the spinal nerves and cord.