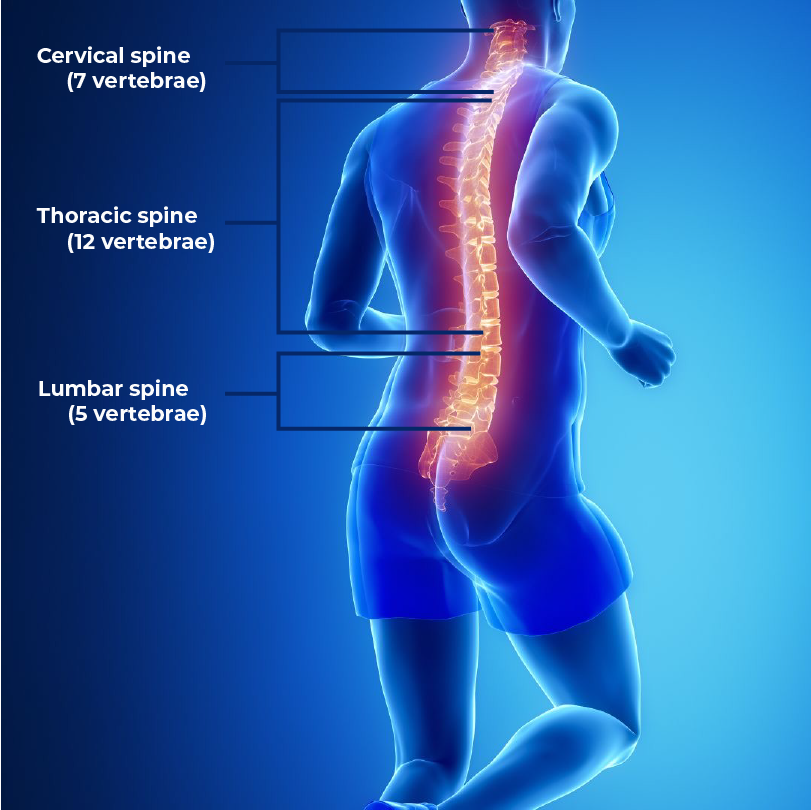
Spine Revision Surgery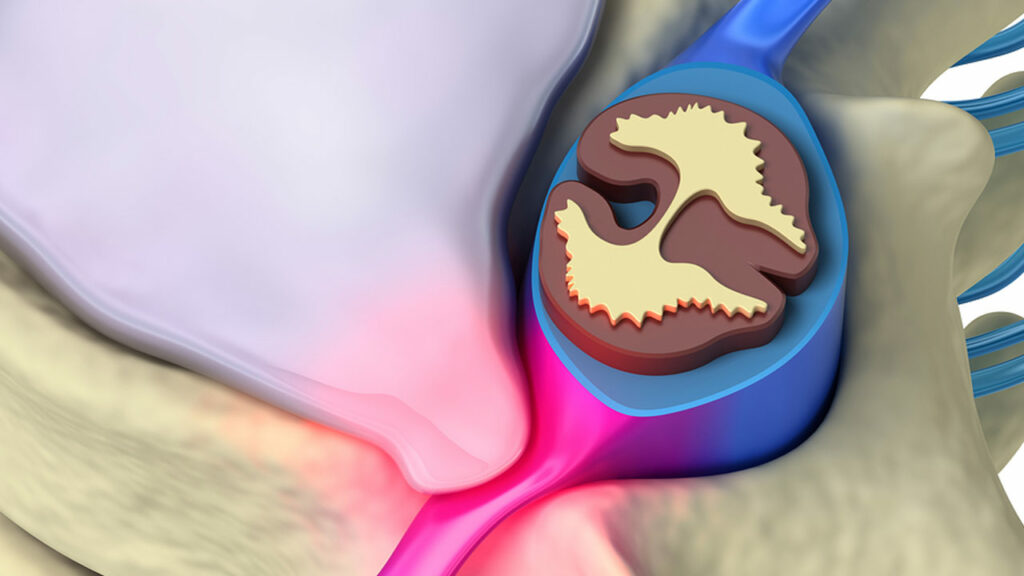
Revision spine surgery is a procedure that takes place on a patient who has already undergone some form of spine surgery. Typically, by three months after surgery, any lingering pain is gone. Revision spinal surgery is sometimes considered when a patient is still reporting chronic pain beyond this time frame.
Revision surgery may also be related to the re-herniation of a disc, infection, hardware failure, non-surgery-related spine degeneration, flat back syndrome, instability, adjacent segment degeneration, or pseudarthrosis (failure to achieve solid fusion).
Indications You Might Need Revision Spine Surgery
When issues continue following back or spine surgery, revision spinal surgery may be needed to address them. This does not imply that something went wrong with the initial surgery, but rather that it frequently requires time and several tries to address the complicated and evolving problems with the spine.
However, if you are experiencing pain or other discomfort well after your initial surgery, you may need to consider revision surgery. Common symptoms included:
- Persistent or chronic discomfort
- Shooting pains in the arms, neck, or back
- Extreme pain that is intense, burning, tingling, or piercing
- Numbness or a lack of sensation
Revision spinal surgery is reserved for individuals who continue to endure chronic pain following surgery and is used in some patients to address or revise issues that were unresolved in prior spine procedures.
Failed Back Surgery Syndrome (FBSS)
The term “failed back surgery syndrome,” also known as “FBSS” or “failed back syndrome,” is misleading because it does not refer to a syndrome. Rather, it is a general term frequently used to describe the condition of patients who have undergone back or spine surgery but did not experience a successful outcome, including continued to experience pain afterward. In any other operation, the phrase “failed back surgery syndrome” does not exist, e.g., no failed cardiac surgery syndrome exists.
There are various reasons why a back operation might or might not be successful, and even with the best surgeon and for the best cases, the success rate of spine surgery is just 95% at best.
Causes of Failed Back Surgery Syndrome
Three main things can be accomplished with spine surgery:
- Decompress a compressed nerve root
- Stabilize a painful joint
- Both of the above
Unfortunately, spine surgery cannot eliminate patients’ discomfort every time. The anatomical injury or root cause that is most likely the source of back pain must be found and correctly diagnosed before spine surgery can be successful.
 However, there are still additional reasons for revision spinal surgery, such as:
However, there are still additional reasons for revision spinal surgery, such as:
- Complications from previous surgery, such as fibrosis or the formation of scar tissue after surgery
- Cauda-Equina-Syndrome (CES)
- Progressive deformities like scoliosis and osteoporosis can worsen over time
- Failure of the spine to fuse following surgery
- Radiculopathy as indicated by difficulty holding things, bladder, or bowel problems
- Walking or balance issues
- Repeated herniated discs
- Incorrect diagnosis
- Prior illnesses that increase the risk of surgical complications and decrease the likelihood of a favorable outcome
- Surgical error
- Failure or malfunction of spinal hardware or implants
Additionally, a patient’s lifestyle and other health issues may be the reason for a failed spine operation.
Smokers are more likely to experience unsuccessful spine surgery. Why is that so? You undoubtedly already know that cigarette smoke contains harmful substances. For instance, nicotine interferes with the body’s capacity to repair bones. The bones may not join properly if someone has spinal fusion surgery and keeps smoking. Smoking contributes to an increased risk of bleeding and infection.
Naturally, smoking isn’t the sole factor in spinal procedures gone wrong. People with autoimmune diseases, peripheral vascular disease, obesity, and diabetes may also be more likely to experience difficulties following surgery.
What Are The Risks of Revision Spine Surgery?
Any surgical procedure carries the possibility of complications. These complications, if they arise, can be serious when surgery is performed close to the spine and spinal cord. Possible complications include the need for additional surgery as well as lingering pain and disability.
The risks of surgery should be discussed with your surgeon before the procedure. The list of potential complications offered here is not meant to be comprehensive, and it is not a replacement for talking to your doctor about the potential risks of surgery.
Risks for surgery in general:
- Infection – There is a chance of infection with any operation. However, less than 1% of spinal procedures get infections. An infection may only affect the skin incision or spread deeper to affect the vertebrae and the regions around the spinal cord. To avoid infections, surgeons take all necessary precautions. Antibiotics will be administered to you just before surgery, especially if a bone graft, metal screws, or plates will be used in your procedure. If a wound gets red, swollen, does not heal, or is hot, these are signs of infection. Call your surgeon immediately.
- Complications from anesthesia – Most spinal surgeries are done under general anesthesia. General anesthesia may cause complications in a very small number of individuals. Adverse drug reactions, issues with your existing medical conditions, or issues with the anesthesia may bring out these issues. Talk to your anesthesiologist about these rare but important complications.
- Breathing issues – If you had general anesthesia and were intubated, you want to ensure your lungs function fully after surgery. Poor oxygen flow, exacerbated by lying in bed, can slow healing and increase the risk of pneumonia. Deep breathing exercises ensure your lungs get the oxygen they need to function properly.
- Thrombophlebitis – is an inflammatory response that mainly affects the legs resulting in a blood clot forming and blocking one or more veins. The afflicted vein may be deep within a muscle or close to the skin’s surface (superficial thrombophlebitis) (deep vein thrombosis, or DVT). Thrombophlebitis may be brought on by trauma, surgery, or extended inactivity. The risk of developing DVT is much higher following surgery involving the pelvis and the lower extremities.
- Mechanical – Blood that is flowing has a lower chance of clotting. The best way to prevent DVT is to move around so that your blood circulates better. Other activities can be performed in bed to improve blood flow from the legs back to the heart. Simply pumping your feet up and down (as if pressing on the gas pedal) tightens the calf muscles, constricts the veins, and forces the blood back to the heart. You cannot practice this enough. The same issue occurs with pulsatile stockings, which use a pump to inflate the stockings.
- Medical – Medications that slow down the body’s clotting process are frequently administered to lower the risk of DVT. Simple aspirin is one of these medications, used in conditions with minimal risk, and heparin injections may be used in high-risk situations.
Often, spinal surgery combines mechanical and medicinal techniques. Using pulsatile stockings immediately following surgery, having you start exercising right away, and getting you out of bed as soon as possible. Giving you medicine to decrease the blood clotting process is a standard procedure for many surgeries.
Risks specific to spine surgery:
- Spinal Cord Injury – There is a small chance of spinal cord damage whenever the spine is operated on. Serious injury to the nerves or the dura, the covering of the spinal cord, may result. Specific sections of your body are connected to the nerves in each vertebra in the spinal cord. Depending on which spinal neurons are impacted, damage to the spinal cord can result in paralysis in some locations but not others.
- Persistent Pain – Sometimes, spinal procedures are not successful. Not all pain may be relieved following spinal surgery, one of the most frequent side effects. Before surgery, be aware of this risk and talk with your physician. They will be able to offer you a sense of the relief you can anticipate. Although some discomfort following surgery is expected, you should inform your doctor if the discomfort persists weeks after the procedure.
- Hardware Fracture – Hardware, such as screws, discs, or plates, can occasionally break or shift out of place before your operation has fully healed. A “hardware fracture” can happen. If this occurs, it might be necessary to do a second operation to replace or remove the hardware.
- Sexual Dysfunction – The nerve signals that enable the rest of your body to operate, experience sensation, and even have sex are carried by the spinal cord and spinal nerves. Numerous issues can arise from damage to the spinal cord and surrounding nerves. A damaged nerve entering the pelvic area may lead to sexual dysfunction. Although this is not a common issue, if your surgery is for your lower back, you may wish to discuss it with your surgeon.
- Pseudoarthrosis (false joint) – Pseudo means false, and arthrosis is a joint condition. Pseudoarthrosis is the medical word for a fake joint. A surgeon uses this phrase to refer to either a broken bone that has not healed or an unsuccessful effort at fusion. A pseudoarthrosis typically indicates that the two bones that should be fused or healed are still moving relative to one another. There is typically ongoing discomfort when the vertebrae involved in a surgical fusion do not heal and fuse. Pain can get worse with time and can necessitate additional surgery. Your surgeon may place an additional bone graft or change the metal hardware to encourage the fusion to heal.
- Implant Migration – The phrase “implant migration” refers to the fact that the implant has moved from the initial location where the surgeon inserted it. This typically occurs very soon after surgery before the healing process has advanced to where the implant is firmly bonded by bone development or scar tissue. Your surgeon can determine if your implant has moved with an x-ray.
If You Are Considering Revision Spine Surgery – Thoughts To Consider
You might wonder what you can do to increase the likelihood that revision surgery will be successful, given you suffered an unsuccessful back surgery. Being an informed and involved patient will help you achieve better results even when some circumstances are beyond your control.
How can you impact your future results? Before your procedure, the place to start is by asking your surgeon questions like the ones below.
- Are there any less invasive spine surgery or spinal cord stimulation methods I have not examined for my problem as alternatives to more spine surgery?
- What are the advantages and disadvantages of this process?
- What is the success rate of the procedure for my back surgery revision?
- What dangers do I run if I don’t get this treatment?
We want you to feel confident about having revision surgery after a failed back procedure. You can then choose a course of action that supports your best interests by being aware of the options, risks, and advantages as they apply to you.
Before Surgery – Diagnosis and Testing
Receiving an early, accurate diagnosis of your issue is one of the most important steps in preventing and treating revision back surgery. This involves:
- Comprehensive assessment of the patient
- Expert knowledge of the affected area and relevant treatment alternatives
- Use of cutting-edge diagnostic imaging equipment
- Understanding the patient’s mental and physical condition, as well as their medical history, must be carefully considered as it may have an impact on the procedure and healing
This will give your surgeon a thorough assessment of the damaged location and the patient’s circumstances to recommend a course of therapy and communicate the necessary preparations for the best outcome.
Your doctor may utilize various diagnostic tools, such as:
- CT scans: Confirm that no new fractures have formed and the bones have fused
- Scans using magnetic resonance imaging (MRI) for localized nerve compression or herniated discs
- X-rays: Check the alignment and hardware integrity
- (EMG) Electromyography Investigate how the nervous system works
- Bone imaging to exclude infection
Recovery From Spine Revision Surgery
How long will it take to recover is the most frequently asked question. Your recovery will rely on various factors, including your general health, the severity of your pre-surgery symptoms, and the type of procedure you underwent. For example, a spinal fusion connects two discs. Your backbone can recover in six months to a year. A small amount of spine tissue is removed during a laminectomy or discectomy. You might feel better in a month. Whatever procedure you underwent, caring for your back after surgery typically involves the same basic steps.
Going Home
Preparing your home – You need to arrange your home in advance for ease of use to avoid reaching, stretching, or straining:
- Move everyday things with easy reach
- Have your prescriptions filled before your surgery
- Ensure you have access to plenty of fluids
- Plan or prepare healthy meals in advance or have someone on hand to cook. Eat fresh, wholesome foods low in salt and preservatives
- Consider installing gripper bars in the bathroom near the toilet and the shower
- Put a riser on your toilet seat to get up without effort
- Slip-on shoes and elastic waistbands are helpful in the beginning
- Have a stool or chair in the shower. NOTE: You have to keep the incision dry for several days, so follow your surgeon’s aftercare instructions
Pain control – You were given a prescription for painkillers when you left the hospital or by prescription before your surgery. To avoid pain, take your medication on schedule to prevent pain before it gets too much. You might want to time your medication to take at least 45 minutes before a physical therapy session. Following surgery, doctors advise stopping narcotic medications as soon as possible due to their addictive nature.
Before and right after spinal surgery, refrain from using ibuprofen, aspirin, or other NSAIDs until your surgeon tells you it is safe to take them, as these medications may hinder healing.
Sitting – After physical therapy, it could be appealing to relax in a cushy chair and watch TV for a while but resist the urge. Choose a substantial chair with arms instead. You want to maintain a straight back and good posture. Alternate your positions but be cautious to avoid twisting your spine. Periodically, while sitting, move your ankles and feet up and down to help your legs’ blood flow. After 30 to 45 minutes of sitting, go for a short walk, even if it’s just around the house, to get your blood circulating.
Sleeping – The healing process depends heavily on quality sleep. But to safeguard your spine, make sure to sleep in the right postures:
- Put a pillow beneath your head and legs if you prefer to sleep on your back
- Put one under your head and one between your knees if you prefer to sleep on your side
- Do a log roll when you get out of bed. Roll to one side while bending your knees, then push up with your arms
If you can nap every day, that will aid your body’s recovery.
Physical therapy – You must continue your spine-strengthening practices after you leave the hospital. Your doctor will determine the frequency of your physical therapy visits. One of the main workouts is walking. You’ll heal more quickly the more you walk and decrease the risk of a blood clot. Some patients need a walker or cane for temporary assistance and safety while undergoing physical therapy.
Back to work – The surgery you underwent and the type of employment you do will determine when you return to work. After surgery, you shouldn’t do too much too soon. The initial recovery process could take a few weeks or as many as three months. For example, you have to twist your spine to check your blind areas and mirrors. To drive, you must stop taking narcotic painkillers and obtain your doctor’s approval. If you work virtually, you may be able to return to some of your duties sooner.
A lot of patients begin routine activities about three weeks after surgery. It is helpful to understand what to expect during recovery so you can convey to your employer when they can expect you to return to some or all of your job responsibilities.
Follow-up after surgery – After your operation, you’ll visit your doctor again somewhere in the first 2-6 weeks, depending on your surgery. Your surgeon will want you to follow up over the next few months, up to two years.
Imaging tests, such as X-rays or MRIs, may be performed to determine how well your back is recovering. Ask your doctor if anything might help make you more comfortable and safer when you return to work. For instance, if you work at a desk all day, a swivel chair may be helpful to prevent twisting of your spine. You may need to take frequent breaks to walk to keep your circulation flowing. All of these considerations and others should be discussed with your surgeon and employer before returning to work or resuming the responsibilities of caring for children and a household.
If it’s time to explore your options, contact SA Spine for your initial appointment and begin the journey to pain relief.

