What Is A Diskectomy?
A Diskectomy is a surgical procedure to remove a damaged portion of a herniated spinal disk. A herniated or collapsed disk irritates or compresses nearby nerves. A Diskectomy is most effective for treating the type of pain that radiates down your legs or arms (otherwise known as radiculopathy) but can be beneficial for any of the three areas of the spine:
-
-
- Lumbar or lower back radiculopathy
- Thoracic, upper and middle back radiculopathy
- Cervical or neck radiculopathy
-
The procedure is not generally helpful for treating back pain or neck pain. People with back or neck pain often find relief with physical therapy and other more conservative treatments. However, in some cases, a surgical procedure may be warranted. Your doctor may refer you to a spine surgeon for a diskectomy if more conservative, nonsurgical treatments have not worked or if your symptoms do not improve or even worsen.
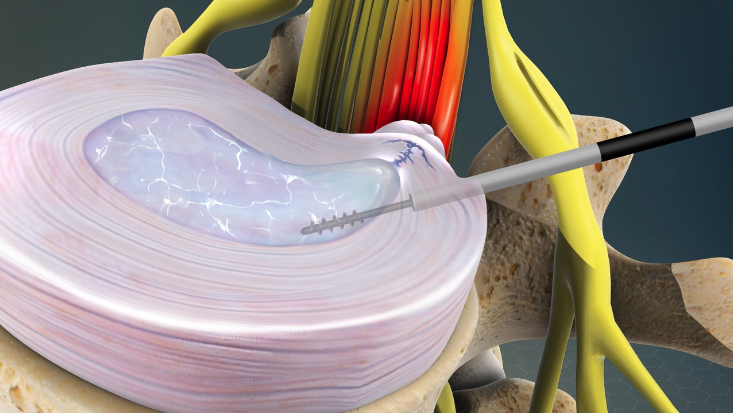
There are several methods to perform a diskectomy. Many surgeons use a minimally invasive technique to perform a diskectomy. A minimally invasive approach uses a small incision and a microscope for viewing the procedure internally.
Why Is A Diskectomy Done?
A diskectomy may be necessary to relieve the pressure of a herniated disk on a spinal nerve. Your doctor may have also referred to this condition as a slipped, prolapse, bulging, or ruptured disk. A herniated disk happens when the soft nucleus at the center of the disk pushes out through a tear in the more rigid rings on the perimeter of the disc. Because the nerves sit in the spinal canal behind the disc, when the disc material herniates into the spinal canal, it pinches the nerves.
In the early stages, disc herniation also causes extreme inflammation of the nerves due to chemical irritation from inflammatory substances in the disc. The nerves are like electrical wires to your arms and legs. When they are irritated or compressed, the result is numbness, tingling, pain, or weakness. You can even lose your proprioception (the ability to sense where your limbs are in space).
When do doctors recommend diskectomy?
-
-
- Pain radiates into your buttocks, chest, arms, or legs and becomes too intense to manage.
- More conservative treatments, like physical therapy or steroid injections, fail to improve your symptoms after several weeks of therapy.
- Your arms or legs become dramatically weak, causing you to drop things, trip when you walk, etc.
- Standing or walking is difficult due to nerve weakness.
-
Risks
It is good to know that a Diskectomy is considered a relatively safe procedure. Keep in mind, as with any surgery, a diskectomy carries potential risks and complications.
Potential complications include:
-
-
- Infection
- Bleeding
- Injury to nerves or blood vessels in the spine
- Leaking spinal fluid
- Persistent symptoms
-
You can minimize the risk of complications by doing your research before choosing a surgeon. When you have your first appointment, here are examples of several questions you might ask to assess if a surgeon is a good fit for you:
-
-
- How long have you been performing this procedure, or how many have you done?
- What method do you use to perform this procedure (more or less invasive)?
- What results do your patients report after surgery, especially relating to pain relief?
- Do you have patient reviews I can read?
- What are my preoperative and postoperative restrictions?
-
Patient confidentially prohibits doctors from revealing patients’ names and medical procedures, but third-party reviews are an excellent source of a doctor’s results from their patient’s point of view.
How You Prepare For Your Diskectomy
Your surgeon will provide specific instructions, but here are examples of the most general preparations:
-
-
- Before spine surgery, stop taking blood-thinning medications and supplements (per your doctor’s instructions).
- No food or liquids for a prescribed time before surgery and anesthesia (usually 8 hours before surgery)
- You may want to consider that there will be restrictions on your movements right after surgery and arrange frequently used objects within easy reach.
- You should limit your activity to walking and lifting to 5 lbs. for the first 6 weeks to avoid a recurrent herniation (Each doctor has a different protocol so be sure to consult with your surgeon about their restrictions).
- Slip-on shoes are a simple but easy way to avoid bending down the first few days.
- Nutrition is essential to healing. If you do not have someone to make your meals the first few days, you may want to pre-prepare a few meals that you can quickly heat.
- Quality sleep is critical for healing. Make sure your bed, pillows, and sleeping environment are conducive to quality sleep. If you are a light sleeper or it takes a long time to fall asleep, experiment with some soothing sleep apps that help ensure deep sleep.
- Stop smoking two months before surgery. Not only does smoking significantly increase how much and how long you bleed, but it also increases the risk of infection and accelerates the degeneration of your spinal discs, leading to more pain.
-
What Should I Expect
During your Diskectomy
The majority of surgeons perform a diskectomy under general anesthesia. This provides the most comfort for the patient and allows the doctor to give their complete focus to your procedure.
During the surgery, small amounts of the spinal bone and ligament over the nerves may need to be removed to give your surgeon access to your herniated disk.
In the ideal surgery, only the fragment of the disk pinching the nerve is removed. The goal is to relieve the pressure but leave most of the disk in place to provide adequate padding between your spinal bones.
If your spine is unstable due to the disc becoming incompetent, you will likely need a fusion to stabilize your spine. This can be determined by performing X-rays in which you bend forward and backward to identify excessive shifting of the bones. In the event you need a fusion, your surgeon may fill the space with:
-
-
- Bone from a cadaver (Dr Cyr’s preference)
- A synthetic spacer (cage)
-
The adjoining vertebrae are fused with metal components in this more in-depth surgery
After My Diskectomy
Once your spine surgery is complete, you will be moved to a recovery room where your healthcare team observes your recovery to watch for complications from anesthesia or surgery and ensure you are comfortable.
You may be able to go home the same day you have surgery, although a short hospital stay may be advised if you have pre-existing medical conditions, or your surgery is more extensive.
Returning to daily activities and work will depend on how much sitting, walking, and lifting you do—plan on returning to work in two to six weeks based on your doctor’s lifestyle assessment. For example, if your job includes lifting heavy objects or operating machinery, your surgeon may advise a six-to-eight-week recovery before returning to work.
One of the most important aspects of healing and recovery from spine surgery is getting enough good quality nutrition, sleep, and movement. Walking, even around the house, increases blood flow, helps to reduce swelling, and prevents blood clots from too much inactivity.
Results
A Diskectomy reduces or eliminates the symptoms of a herniated disk for most people with nerve compression resulting in radiating pain.
However, a Diskectomy may not be a permanent fix if it doesn’t address the source that caused the disk to become herniated. It’s essential to avoid re-injuring your spinal disks. Your surgeon may recommend:
-
-
- Weight loss
- A low-impact exercise program
- Limiting activities that involve extensive or repetitive bending, twisting
- Weight lifting limits
-
Dr. Cyr at SA Spine Trained At The Mayo Clinic
You want the best when it’s time to have surgery on something as delicate as your spine. Dr. Cyr completed his Fellowship in Neurological and Orthopedic Surgery Of The Spine at the Mayo Clinic. He was Chief Air Force Spine Surgery and Spine Surgery Consultant to the Air Force and Pentagon Surgeon General. Dr. Cyr taught orthopedic surgery residents, physician assistant fellows, and medical students for six years. Click here to learn more about Dr. Cyr.
See his Contact page to schedule an appointment at one of his offices.