Microdiscectomy Surgery
Note from Dr. Steven Cyr: I do not perform microdiscectomy surgery or other disc replacement surgery as in my medical opinion and experience, these procedures are inferior procedures to fusion. Many articles have shown there’s no substantial advantage to a disc replacement over a fusion, although the theory behind it is commendable. Microdiscectomy surgery has not been shown to improve pain as well as a fusion and doesn’t offer to decrease adjacent level disease better than a fusion procedure. The information below is included so that you, the reader can make an informed decision.
Please note that fusion surgery has a similar profile with superior results.
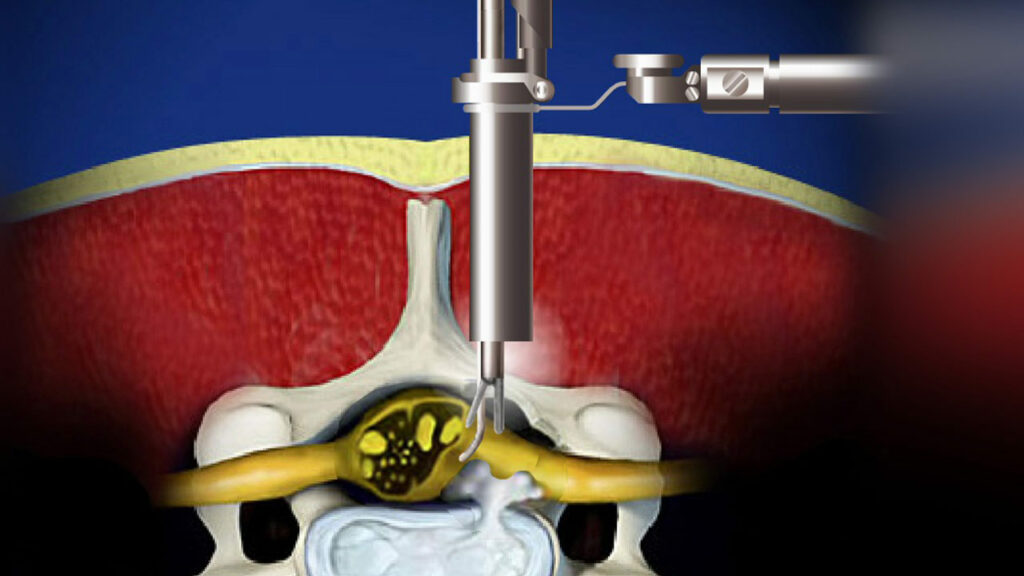
Microdiscectomy surgery, sometimes called micro-decompression, is a minimally invasive surgical procedure performed on patients with a herniated lumbar disc. During this surgery, a surgeon will remove portions of the herniated disc to relieve pressure on the spinal nerve column.
Similar to open discectomies, microdiscectomies are done to remove the intervertebral disc fragment pressing on your nerve and giving you discomfort.
When Is Microdiscectomy Surgery Done?
A microdiscectomy is generally done under two circumstances:
- Your intervertebral disc may have torn or broken, and a piece may be pressing against your spinal nerves or spinal cord
- Your disc is unbroken, but a portion of it may be protruding or bulging and pressing on your spinal nerves or spinal cord
How Is Microdiscectomy Surgery Performed?
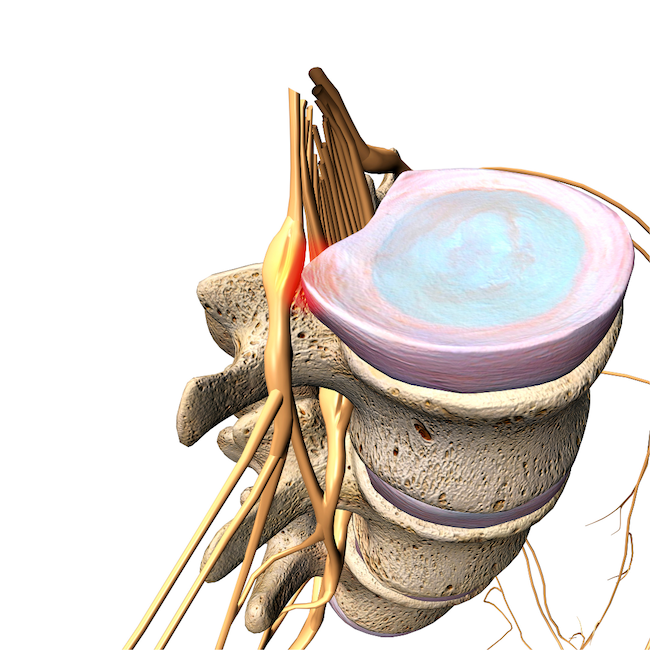
Herniated disc
In microdiscectomy surgery, only a portion of the disc is removed. There are three primary methods for doing microdiscectomies. Microdiscectomies take approximately an hour. Normally general anesthesia is used for this procedure, which is performed lying on your stomach.
Your surgeon will talk with you about the right approach for your best outcome:
Endoscopic: This procedure passes a tiny video camera through a tube to give your surgeon access to your spine so they can use small instruments to remove disc material.
Mini-open: This procedure is comparable to an open discectomy [LINK], but your surgeon views your spine through smaller incisions using cutting-edge technology.
Tubular: Your surgeon makes a modest incision and inserts a tube. Your back muscles are delicately penetrated until it reaches your spine. Expanding tubes are inserted one inside the other. The area where the procedure will be performed is gradually dilated by the tubes. Your surgeon uses devices specially made for this procedure to remove a portion of your disc.
Your surgeon pays close attention to nerve roots and the area around the disc to ensure there are not any additional disc fractured pieces.
Microdiscectomy Surgery Risks
In addition to the usual risks associated with surgery, such as blood loss and infection, microdiscectomy surgery can result in the following complications.
- The disc may herniate again, necessitating additional surgery (fusion)
- Blood vessels, the spinal cord, and nerves are vulnerable to injury
- Discomfort or pain might return
- The disc material was not completely removed during surgery
You should contact your surgeon if you experience any of the following:
- Tingling or weakness in the legs
- Fever
- Loss of bladder control
- Swelling in one or both legs
- Pain in the calf
- Pain that does not resolve with medication
Microdiscectomy Surgery Recovery
The good news is that a microdiscectomy can result in noticeable pain relief and a swift return to your regular life. In most cases, full recovery takes about 12 weeks. Of course, your surgeon will guide you on when you can resume exercising and your regular daily routines. A full recovery is predicated on following best practices for preparing for surgery and your doctor’s aftercare instructions which may include physical therapy.
The First 24-Hours
Even though recovery after microdiscectomy surgery is typically significantly quicker than extensive spine surgeries, it is still a significant operation that requires general anesthesia.
The nursing staff will address that your pain is properly managed once you are awake and in recovery. Nurses will get you up walking and determine that you can urinate.
Microdiscectomies take approximately one hour, and people commonly return home the same day. Your surgeon might recommend staying in the hospital overnight, depending on your circumstances, age, or other medical conditions.
The First Two Weeks
Be prepared for the after-effects associated with major surgery once you are home. Especially in the first few days, pain, low energy, and feeling sleepy are to be expected. Give your body as much rest as it wants but be sure to frequently for your circulation.
Your surgeon will give you detailed aftercare instructions on managing pain and how much exercise you should engage in. Be careful to adhere to these guidelines. However, there are guiding principles after spine surgery. Avoid:
- Bending at the waist
- Lifting objects that weigh more than a few pounds
- Rotating your trunk to the left or right
- Operating a vehicle due to twisting required and taking pain medication
- Long periods of inactivity
Being inactive can exacerbate your discomfort by causing stiffness, swelling, and increasing the likelihood of clots. Mild activity, like walking, goes a long way to keep your body’s lymph and blood circulating.
In most cases, patients can shower 72 hours after surgery. Be sure to follow your surgeon’s instructions, which may vary from the 72-hour window.
Weeks Three to Six
You will undoubtedly notice a considerable increase in energy and a significant decrease in pain after your first two weeks of recovery. Many normal activities can be resumed if you stop using opiate medicines. Most doctors advise not driving until after the second week following your treatment, but in general, you can drive when you stop using narcotic painkillers to manage your pain. It would be best to be cautious about twisting and bending, so consider that when considering activities.
If your profession doesn’t require heavy lifting, long periods on your feet, or manual labor, you can generally go back to work. Ensure your employer is aware that you will need to stand and move about every hour or so during the job. After your surgery, your lower back may be more flexible, but it will get stiff sitting for long periods.
Your incision may still be uncomfortable, and full healing may take longer. Refrain from actions that can pull or strain the surgical area.
Weeks Seven to Twelve
Most patients would resume their regular activities during this time with the help of physical therapy if their doctor prescribed it. This stage of the healing process is crucial for long-term stabilization. With the right exercise, you will get stronger and more flexible. Exercise will support your still-healing spine and aid your posture. Correct posture allows the spine to distribute your weight properly.
Past the two-month mark, you may have the tingles of discomfort but if your recovery has been uneventful, ongoing discomfort will have mostly subsided by this stage.
The most frequently asked question is, “When can I resume all physical activities?” As long as your pain has resolved, patients often resume a variety of sports and physically demanding activities. Your doctor might advise you to refrain from strenuous lifting and other high-impact activities for additional time.
Before returning to certain occupations with heavy physical demands like construction, operating heavy machinery, or patient assistance, you may need a longer convalescence period and additional strengthening exercises.
Back discomfort doesn’t have to be something you “simply live with,” especially if it interferes with your ability to perform everyday tasks and enjoy life. Unfortunately, many people choose to “manage” their pain merely by occasionally using over-the-counter medications to relieve the symptoms. You may be excessively limiting your activity when a microdiscectomy surgery solution would provide the relief that would give you back a fuller life.
FAQ About Microdiscectomy Surgery
What is a lumbar microdiscectomy? A lumbar microdiscectomy is a surgical procedure performed to remove a portion of a herniated disc in the lower back (lumbar region) to relieve pressure on the spinal nerves.
How long does microdiscectomy surgery take? Microdiscectomy surgery typically takes between 1 to 2 hours, although the exact duration can vary depending on the complexity of the case.
What can I expect during the first week after microdiscectomy surgery? During the first week after microdiscectomy surgery, you may experience some pain and discomfort at the surgical site. It’s important to follow your surgeon’s instructions for post-operative care, including rest, pain management, and gentle activity.
How long does a microdiscectomy last? The effects of a microdiscectomy can vary from person to person. In some cases, the relief of symptoms can be long-lasting, while in others, additional treatment may be needed over time.
Is microdiscectomy considered a major surgery? While microdiscectomy is a surgical procedure, it is generally considered minimally invasive compared to traditional open-back surgery. However, any surgical procedure carries some level of risk, and it’s important to discuss the potential risks and benefits with your healthcare provider.
What is the recovery process like during the first week after microdiscectomy surgery? During the first week of recovery, you may need to limit activities that put stress on your back. Your surgeon may recommend gradually increasing your activity level as tolerated while avoiding heavy lifting or bending at the waist.
How does microlaminectomy recovery differ from microdiscectomy recovery? Micro laminectomy and microdiscectomy are both surgical procedures used to treat spinal conditions, but they target different structures of the spine. Recovery from each procedure may vary depending on individual factors and the extent of the surgery.
What is the typical recovery time after microdiscectomy surgery? The typical recovery time varies from person to person but may range from a few weeks to several months. Your surgeon can provide more specific guidance based on your individual case.
Is a discectomy considered a major surgery? Discectomy, including microdiscectomy, is a surgical procedure that involves removing a portion of a herniated or damaged spinal disc. While it is considered a surgical intervention, it is often less invasive than traditional open-back surgery.
What should I expect during recovery from microdiscectomy surgery? You may experience improvements in symptoms such as pain, numbness, or weakness in the legs. However, to optimize your recovery, it’s important to follow your surgeon’s instructions for post-operative care.
How long does microdiscectomy surgery usually take? It usually takes 1 to 2 hours, but the duration can vary depending on factors such as the size and location of the herniated disc.
What is the expected recovery timeline after microdiscectomy surgery? The expected recovery timeline after microdiscectomy surgery can vary, but many patients are able to return to light activities within a few weeks and experience significant improvement in symptoms over the following months.
How long is the microdiscectomy surgery? Microdiscectomy surgery typically takes 1 to 2 hours, but the exact duration may vary based on individual factors and the specifics of the procedure.
Feel free to reach out if you have any further questions or concerns regarding microdiscectomy surgery and recovery.
What’s Next?
 The number of patients who can have a higher quality of life after treatment defines success for Dr. Cyr and all the doctors and medical professionals at SA Spine, a full-service spine and pain clinic. Non-surgical treatment does not always provide significant pain relief. In that case, our patients benefit from surgical procedures provided by world-class surgeons, including Dr. Steven J. Cyr, who trained at the prestigious Mayo Clinic in Rochester, Minnesota.
The number of patients who can have a higher quality of life after treatment defines success for Dr. Cyr and all the doctors and medical professionals at SA Spine, a full-service spine and pain clinic. Non-surgical treatment does not always provide significant pain relief. In that case, our patients benefit from surgical procedures provided by world-class surgeons, including Dr. Steven J. Cyr, who trained at the prestigious Mayo Clinic in Rochester, Minnesota.
SA Spine accepts over 100 insurance plans to prioritize your access to specialty back, neck, and peripheral nerve pain relief. Contact us to make your first appointment and to find out more about our participation in your plan.

