Lumbar Fusion – Percutaneous and Instrumentation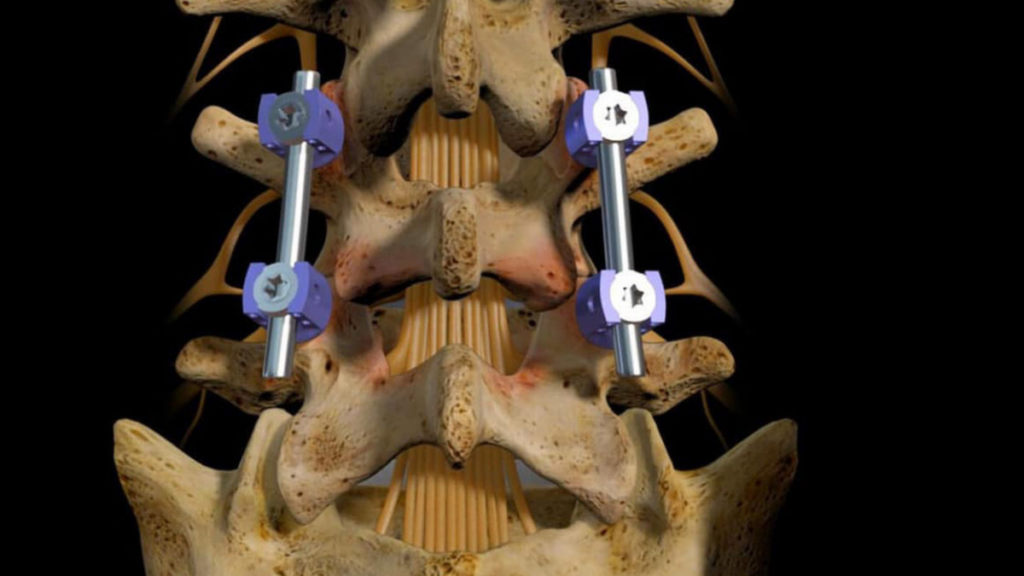
For patients with more serious spinal disorders, vertebrae lumbar fusion is required to immobilize the joints and stabilize the spine. Pedicle screws have been used to fuse vertebrae for a long time, but now this can be done with a “percutaneous” procedure. Instead of open surgery, very small incisions are made in the skin. The surgeon uses X-ray fluoroscopic imaging to guide the placement of the special screws into the vertebrae.
The surgeon then attaches a rod to connect the pedicle screws, stabilizing the spine. This procedure is considered minimally invasive compared to traditional open surgery that splits and retracts the muscle of the spine through a much larger incision.
We cover the information that our patients require and, ultimately, the most Frequently Asked Questions.
What Does Percutaneous Lumbar Fusion With Instrumentation Mean?
- Percutaneous: is a minimally invasive surgical procedure that uses small skin incisions
- Lumbar: the lower back.
- Fusion: a process to “fuse” or create one bone with another
- Percutaneous spinal instrumentation is placing small screws in the spine through a small incision.
Spinal fusion surgery does not “weld” the vertebrae together. Instead, bone grafts are placed where needed on the spine during surgery. The body goes to work and heals the grafts in the coming months. Think of it as the same mechanism as healing a fracture. The screws and rods (hardware/instrumentation) immobilize the joints and stabilize the spine so that the bone graft can heal the bones together.
For patients with more serious spinal disorders, vertebrae lumbar fusion is required to immobilize the joints and stabilize the spine.
Why Might I Need Lumbar Fusion?
Common reasons to perform lumbar fusion surgery are axial or mechanical pain in the lower back. You know if your lower back pain is “mechanical” if it is aggravated by certain activities or positions, like sitting, and if it is better when you rest.
There are also several other circumstances for performing this surgery.
- Spine instability as a result of age, degeneration, infection, or tumor
- Broken or fractured bones as a result of a traumatic injury or accident
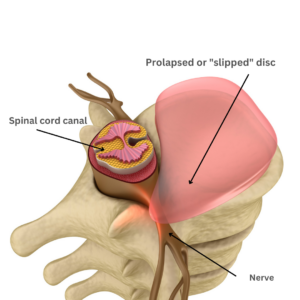
- Back pain as a result of degenerative disc disease
- Conditions like scoliosis that result in an abnormal curvature of the spine
- Long-lasting, chronic lower back pain in some instances
- Spondylolisthesis is when a vertebra slips on the one below, causing pain
Is Lumbar Fusion – Percutaneous and Instrumentation Effective?
While Lumbar Fusion is a common surgery, this particular procedure is only suitable for a specific subset of patients. Many patients come to SA Spine with neck or back pain, but not many need the full lumbar fusion operation.
The success rate for this minimally invasive approach to this surgery using percutaneous spinal instrumentation is around 90 to 95%. Of course, each patient’s success rate depends on their pathology, physiology, weight, and compliance with postoperative restrictions.
Minimally invasive procedures have several advantages:
- Minimal blood loss
- Smaller incisions
- Less scarring
- Lowers the risk of infection
- Less muscular pain after surgery
- Short stay or outpatient
- Faster recovery
- Avoids much of the trauma and possible damage to the back muscles / soft tissue around the spine
Tell Me More About This Surgery
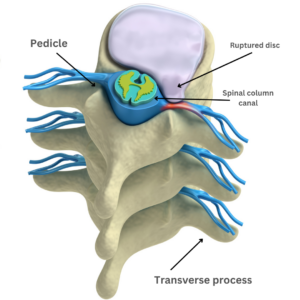
Transverse process and Pedicle
Generally, your surgeon will begin with a small, one-inch incision at the operative part of the spine where there is spinal stenosis or other painful conditions.
A delicate dissection creates space between the transverse processes over the pedicle. The screws are then carefully inserted into the pedicle of the fused bones. X-rays taken during the surgery confirm the placement of the screws. Once the screws are positioned correctly, the surgeon expands the space between them. Often, the disc is removed between the fused bones and replaced by a spacer made of bone or a synthetic cage. This expansion opens up the spinal canal and the hollow archway that creates the channel for the nerves called the foramen and allows the bones to heal in the front and back.
The surgery takes about an hour (per level). Most patients go home the same day as the surgery, but your surgeon will advise you about your case.
Preparing For Your Lumbar Fusion – Percutaneous and Instrumentation
What you do before and after surgery will get you back on your feet more quickly. We cannot stress enough how much patients can impact the successful outcome and speed of recovery by having a good outlook and preparing their environment.
- It’s important to have realistic expectations. Make sure you have weighed all your options and had all your questions answered before deciding to have surgery.
- Prepare properly for your recovery. Get your home ready before surgery.
-
- Move things you often use for easy access so you can avoid bending or reaching.
- Put throw rugs away and move loose cords to remove tripping hazards.
- Prepare and freeze meals or have someone on hand to cook for your first week at home.
- Make sure you have non-slip strips in the shower/tub.
- Installing grab bars in the tub or toilet area can be helpful. If your toilet is too low, get a riser.
- Ensure you have a comfortable height chair with armrests you can easily get in and out of.
- Stop taking NSAIDs (for example, Motrin, ibuprofen, Advil, Naprosyn, Anaprox, Naproxen) 7 to 10 days before surgery as well as any other blood thinners you are taking after conferring with your physician. NSAIDs should not be taken for six months after surgery to add to the healing process. Fusion of the bones is accomplished through inflammation and blood flow; taking these medications diminishes the chance that your bones will heal together.
- Quit smoking at least six weeks before your surgery. Smoking inhibits healing and promotes bleeding.
- Eat a healthy diet of fresh foods vs. processed foods. Not only will that help with healing, but it will also help avoid fluid retention and raised blood pressure.
The bottom line is to think ahead about your restrictions after surgery and prepare for your limited mobility.
Risks / Benefits of Lumbar Fusion
As with any surgery, weighing the risks and benefits is prudent before deciding to proceed. Most patients have tried other non-surgical alternatives like physical therapy, exercise, or pain management. Once other reasonable sources of pain or neurological deficit have been ruled out, it may be time to consider minimally invasive surgery.
Risks
No surgery is without risks, but minimally invasive procedures like Lumbar Fusion – Percutaneous and Instrumentation may have fewer complications than major surgery. These are the risks to know about:
- Infection
- Bleeding
- Blood clots
- Injury to blood vessels or nerves around the site of the surgery
- Pain
Benefits
Do the benefits outweigh the risks? You decide!
- Pain Relief – The most welcome benefit of this procedure is that it frequently provides pain relief.
- Stability– A fusion procedure helps with the strength and stability of the spine.
- Resume activities– For some people, movement is too painful to continue activities they enjoy. Fusion procedures can help you return to some or all physical activities you couldn’t do due to pain.
- Independence– Pain and its limitations can create dependence on others. It’s possible to regain a great deal of your independence with a successful surgery.
- High Success Rate – with the increasing sophistication of minimally invasive spine surgeries, success rates are very high.
Recovery from Lumbar Fusion – Percutaneous and Instrumentation
Early, limited activity once home will speed up the recovery. Staying in bed after surgery is not beneficial. Too much inactivity can lead to problems such as:
- Bed sores
- Pneumonia
- Blood clots in the legs
Understanding the fine line between getting better and doing too much is also important.
- Walking short distances immediately after surgery on level paths is perfect. Avoid hills but start walking 10 minutes twice a day and work up from there.
- Walk upstairs as pain allows.
- Limit pushing and pulling activities like vacuuming, mowing, and mopping.
- Avoid constipation. Pain medications can be constipating. Talk with your doctor about stool softeners or eat extra fiber to prevent straining during bowel movements.
- No lifting more than 5 pounds for several months.
- No driving until your surgeon says it’s safe, and of course, never while on pain medication.
- Your surgeon will guide you on when you can return to work, generally two to four weeks.
- Returning to normal activities varies from patient to patient but plan on limiting activity until your fusion heals (it can take 6-12 months).
When to Call the Doctor
You should expect some pain or discomfort and light bleeding after your procedure. But you need to know when you call your doctor.
Call your doctor immediately if your wound is reddened, swollen, or drains fluid. If you have swelling or pain in your legs, shortness of breath, or anything concerning, go to the nearest ER or call 911.
What’s Next?
Steven J. Cyr, M.D., is a Board Certified Orthopedic Surgeon who received extensive training to specialize in the delicate science of Spine Surgery. Anyone who knows Dr. Cyr well will tell you that he is a man driven by quality and excellence. His high standards can be seen throughout his educational process and career.
Start your journey to relieve your pain and increase your mobility with a consultation.
Frequently Asked Questions
Patients ask many of the same questions when they come for their first appointment and prepare for their procedure. Here are some of the most common concerns:
Is Lumbar Fusion – Percutaneous and Instrumentation painful?
Any surgery is painful, but with minimally invasive surgeries, muscular pain tends to be less. Your surgeon will ensure your comfort with pain medication for the first days after your procedure.
Will the procedure stop the pain I am experiencing?
Spinal fusion is not guaranteed to relieve all your pain. However, this fusion surgery has a high success rate in relieving most or all of the pain you are currently experiencing.
Is Lumbar Fusion – Percutaneous and Instrumentation surgery an inpatient or outpatient procedure?
This is a minimally invasive procedure; most patients go home the same day. Depending on your overall health, and how many areas your surgeon addresses, your surgeon may want you to stay overnight in the hospital for a night or two.
What type of anesthesia is used during my procedure?
Surgeons perform spinal fusion surgeries under general anesthesia. You will be unconscious during the procedure.
When Can I Shower?
Your incision will be covered by gauze and a bandage. If your surgeon uses an “op-site” bandage, it is waterproof, allowing you to shower about 48 hours after your surgery. But if there is white tape over the wound, wait five days to shower. Dressing changes with sterile gauze should begin on postoperative day 3. However, DO NOT submerge your bandage or surgery site underwater for six weeks, or you will risk infection. No baths, pools, or hot tubs until your surgeon lets you know you can resume those activities- typically six weeks.
What Can I Do to Speed Recovery?
This is one of the most important questions for patients who want to return to more normal activities sooner.
- Movement is essential for your body’s circulation and lymph fluids. Short, frequent walks are ideal
- Eat a healing diet of fresh foods and quality proteins
- Sleep is essential for healing. If you need to take a mild sleep aid to get quality sleep, talk with your surgeon
- Prepare your home for easy use
- Get help the first week to two
- Get mobility training if appropriate
Ready to make an appointment to discuss your surgical options? Click here.

